Junk Food Binge May Alter Brain Insulin Response
TOPLINE:
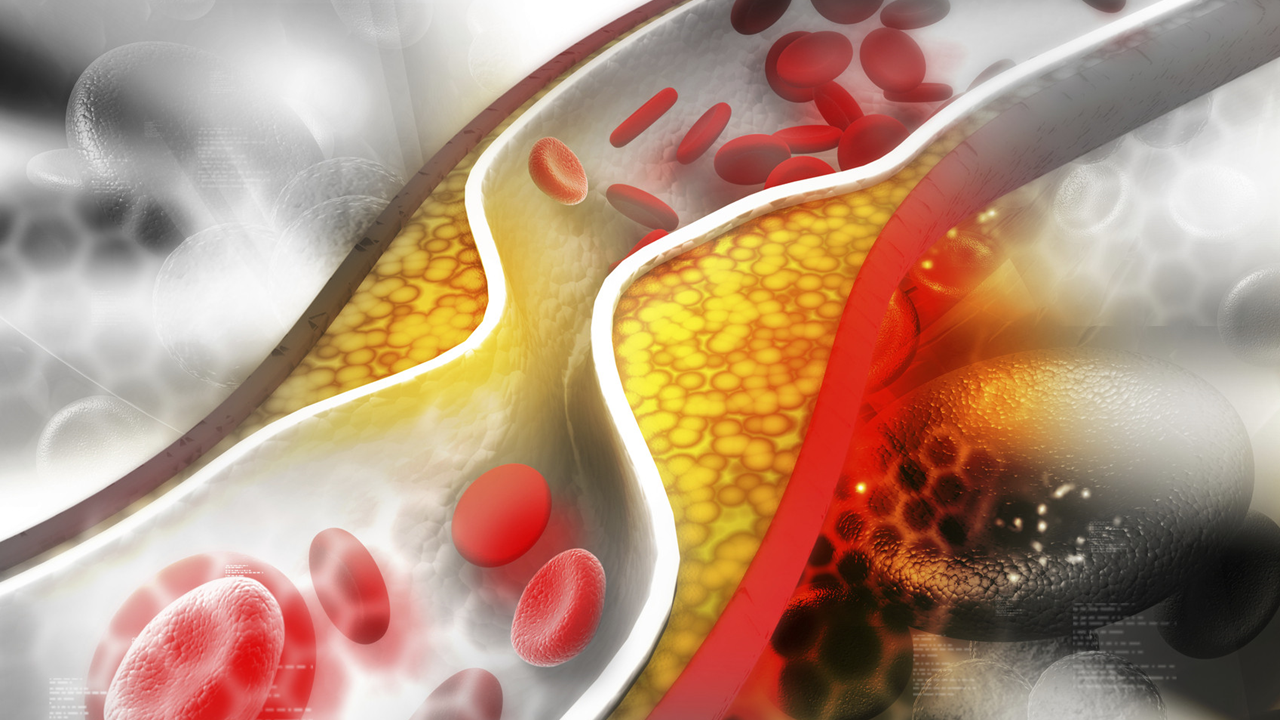
A 5-day high-caloric diet triggered liver fat accumulation and disrupted brain insulin action in men with a healthy body weight, with effects persisting even after resuming a normal diet. Researchers postulated that brain insulin responsiveness may adapt to dietary changes before weight gain, potentially facilitating the development of obesity.
METHODOLOGY:
- In healthy individuals, insulin signaling in the brain controls appetite and food intake, but in insulin-resistant states, this regulation is impaired, leading to increased visceral fat, poor metabolism, and greater fat regain after lifestyle changes.
- Researchers examined the effect of a 5-day high-caloric dietary intervention that incorporated widely available calorie-rich, ultraprocessed snacks alongside a regular diet on brain insulin action, body fat composition, and peripheral insulin sensitivity.
- They enrolled 29 male volunteers aged 19-27 years with a body mass index of 19-25 and assigned 18 participants to a high-caloric diet group and 11 participants to a control group receiving a regular diet.
- Participants in the high-caloric diet group consumed an additional 1500 kcal/d for 5 consecutive days before the first follow-up visit and then returned to their normal diet for 7 days prior to the second follow-up visit.
- Brain-specific effects of insulin action and fat content in the liver were assessed using MRI.
TAKEAWAY:
- Liver fat content significantly increased at the first follow-up visit in the high-caloric diet group (P = .005); however, no such effects were observed in the regular diet group. Body weight, peripheral insulin sensitivity, or inflammatory markers were not different between the groups.
- Participants in the high-caloric vs regular diet group showed significantly higher insulin activity in the right insular cortex, left rolandic operculum, and right midbrain/pons regions during the first follow-up visit (whole-brain corrected Pfamily wise error < .05).
- After 1 week of resuming a regular diet, the high-caloric diet group demonstrated significantly lower brain insulin activity in the right hippocampus and bilateral fusiform gyrus than the regular diet group (whole-brain corrected Pfamily wise error < .05); the reduced insulin responsiveness in the fusiform gyrus was linked to reported changes in carbohydrate intake, and changes in hippocampal insulin responsiveness correlated with variations in fat and saturated fatty acid intake.
- Compared with participants in the control group, those in the high-caloric diet group showed reduced reward sensitivity (Pboot < .001) and increased punishment sensitivity (Pboot = .002) after just 5 days of consuming calorie-rich, ultraprocessed snacks.
IN PRACTICE:
“We show that short-term overeating with commonly used ultra-processed high-caloric snacks can trigger liver fat accumulation and short-term disrupted brain insulin action that outlast the timeframe of the HCD [high-caloric diet] in men,” the study authors wrote.
SOURCE:
This study was led by Stephanie Kullmann, PhD, Institute for Diabetes Research and Metabolic Diseases, Helmholtz Center Munich, University of Tübingen, Tübingen, Germany. It was published online in Nature Metabolism.
LIMITATIONS:
The small sample size was a major limitation of this study. Whole-body insulin sensitivity was not assessed using the gold standard method (hyperinsulinemic-euglycemic clamp). The study investigated male participants exclusively, making it unclear whether the findings extend to women, particularly given known sex-specific findings of insulin action on appetite, metabolism, and memory that depend partly on the menstrual cycle.
DISCLOSURES:
The studies received partial support through a grant from the Federal Ministry of Education and Research to the German Center for Diabetes Research and a grant from the State of Brandenburg. One author reported receiving research grants and lecture fees from and having other ties with many pharmaceutical companies.
Source
Bài viết liên quan